Medication List Checklist
Ensure you have everything critical for your medication safety with this checklist. Missing just one item could lead to dangerous errors.
Every year, more than 1.5 million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t caused by bad doctors or faulty prescriptions. They happen because someone didn’t know what they were taking - or worse, their doctor didn’t know either. A simple, updated medication list can stop most of these mistakes before they start.
Why Your Medication List Matters
You might think your doctor has all your medication info. But they don’t. Not really. Hospitals and clinics rely on what you tell them - not what’s in their system. A 2020 study by the Agency for Healthcare Research and Quality found that nearly half of all medication errors during hospital transfers happened because the patient’s list was wrong or missing. That’s not a glitch. It’s a system gap. And you’re the only one who can fill it. Your list isn’t just for emergencies. It’s for every doctor visit, every pharmacy refill, every time you see a new specialist. It’s your safety net. When you’re in pain, confused, or too tired to explain, that piece of paper or phone app could save your life.What to Put on Your Medication List
A good medication list doesn’t just say "I take blood pressure pills." It tells the full story. Here’s exactly what you need to include:- Brand and generic names - Write both. If you take Lisinopril, also write "Zestril" or "Prinivil." Some pharmacists only recognize brand names.
- Dosage and strength - Not "one pill a day." Write "10 mg once daily." If you take 5 mg in the morning and 10 mg at night, write that too.
- Why you take it - "For high blood pressure" or "for arthritis pain." This helps providers spot duplicates or unnecessary meds.
- When and how to take it - "Take with food," "take on an empty stomach," "take at bedtime." Even small details matter.
- Over-the-counter drugs - Tylenol, ibuprofen, antacids, sleep aids. These are the most common missing items. One study found 30% of adverse reactions happened because OTC meds weren’t listed.
- Vitamins and supplements - Fish oil, magnesium, vitamin D, herbal blends. These aren’t harmless. Some interact badly with blood thinners, heart meds, or chemotherapy.
- Allergies and bad reactions - Not just "allergic to penicillin." Write what happened: "Rash after amoxicillin," "swelling after sulfa drug."
- Emergency contacts - Name, phone, relationship. If you can’t speak, someone else needs to tell providers who to call.
Some people even add the pill’s physical details: color, shape, imprint code. If you’re ever in a hospital and your meds are taken away, this helps staff identify them quickly.
How to Keep It Accurate
A list that’s outdated is worse than no list at all. The CDC says 35% of medication errors come from outdated records. Here’s how to keep yours current:- Update it the same day - If your doctor changes a dose, stops a drug, or adds a new one, update your list immediately. Don’t wait.
- Use one method - Paper, app, or both. But pick one and stick with it. If you use paper, keep a copy in your wallet and another at home. If you use an app, make sure it syncs across devices.
- Use the same pharmacy - CVS, Walgreens, or your local pharmacy. When you use one place for all prescriptions, they build a complete record and can flag dangerous interactions.
- Take photos of your pills - Snap a picture of each bottle or blister pack. Store them in a folder on your phone. This helps if you lose the list or need to show a provider what your meds look like.
- Write notes on the bottle - Stick a small label on your pill bottle: "For back pain" or "Take with breakfast." It’s a backup if you forget.
There’s even a new trick: some pharmacies now let you scan the barcode on your pill bottle with an app, and it auto-fills your list. The University of Michigan tested this in 2023 and cut documentation errors by 63% in older adults.
Who Should See Your List
Don’t keep it to yourself. Share it with everyone involved in your care:- Your primary doctor - Bring it to every appointment.
- Your pharmacist - They’re trained to spot interactions. Ask them to review it quarterly.
- Specialists - Cardiologists, neurologists, pain clinics - they all need to know what else you’re taking.
- Dentists - Some antibiotics and pain meds interact badly with heart or blood pressure drugs.
- Physical therapists - If you’re on muscle relaxants or sedatives, they need to know your balance or alertness might be affected.
- Family or caregivers - Especially if you live alone. Make sure someone knows where your list is and how to use it.
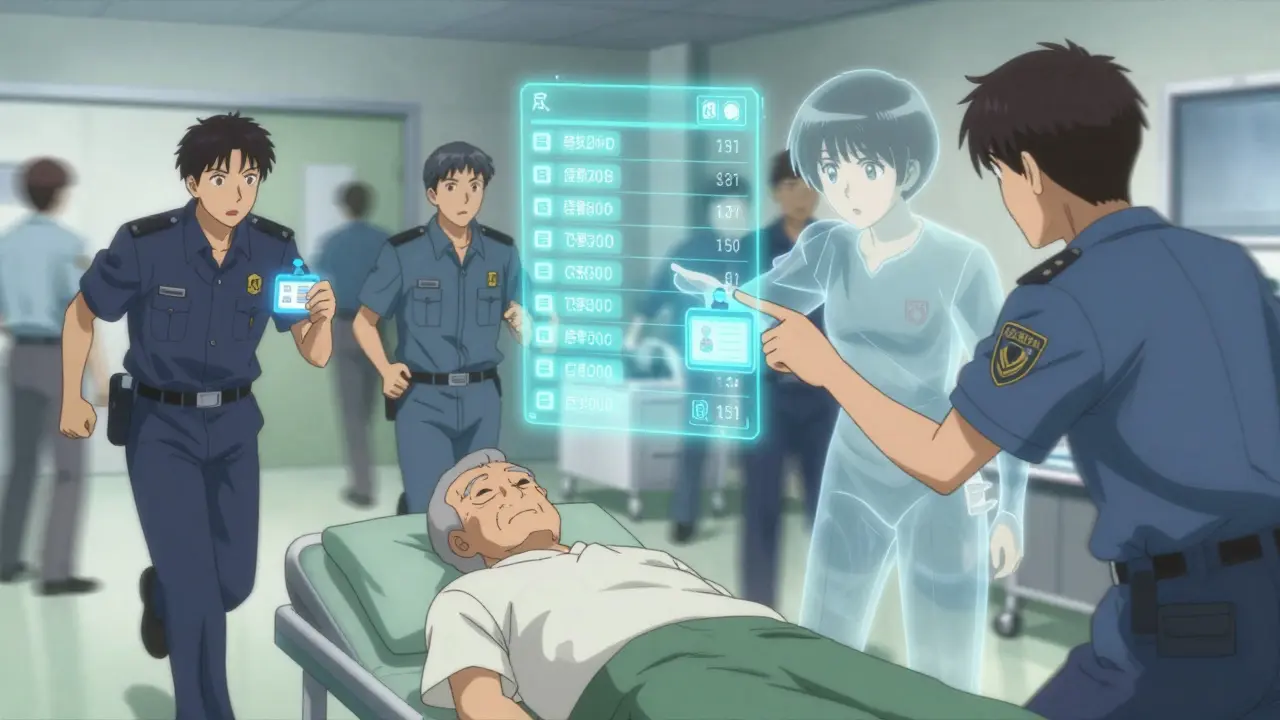
Emergency responders don’t have time to guess. If you’re unconscious after a fall, the paramedic’s first question is: "What medications is this person on?" If you’ve got a card in your wallet or a digital list on your phone, they get the answer in seconds.
Technology Can Help - But Don’t Rely on It Alone
There are apps like FDA’s MyMedSchedule, GoodRx, and Medisafe that let you scan pills, set reminders, and share lists. The FDA’s app now uses photo recognition to identify pills with 92% accuracy. But here’s the catch: 62% of adults say they have a medication list, but only 28% keep it updated. Technology is a tool - not a replacement for personal responsibility. If your phone dies, your app crashes, or you forget to sync it, you’re back to square one. That’s why the CDC and FDA still recommend carrying a printed copy.Who Benefits the Most?
Older adults are at highest risk. The CDC says adults 65+ take an average of 4.8 prescription drugs - and 40% take five or more. That’s a lot of chances for something to go wrong. Add in supplements, OTC meds, and over-the-counter sleep aids, and you’ve got a cocktail that can throw off your balance, memory, or heart rhythm. But it’s not just seniors. Anyone taking more than three medications regularly - whether for diabetes, depression, asthma, or chronic pain - should have a list. Even if you’re young, if you’re on birth control, antidepressants, or painkillers, your list matters.What Happens When You Don’t Have One
Imagine this: You’re in the ER after a fall. You’re confused. You can’t remember your meds. The doctor orders a new painkiller - one that interacts with your blood thinner. You bleed internally. It’s preventable. Or you get admitted for pneumonia. The nurse gives you a sedative. You’ve been taking melatonin for sleep. The combination knocks you out. You stop breathing. It’s rare - but it happens. These aren’t hypotheticals. They’re documented cases. The FDA and CDC track them. And they all point to one thing: accurate medication lists save lives.Start Today - Here’s How
You don’t need to be perfect. You just need to start.- Grab a piece of paper or open a notes app.
- Go through your medicine cabinet. Write down everything you take - even the ones you only use once a month.
- Call your pharmacy. Ask them to print out your full prescription history.
- Compare the two lists. Add anything missing.
- Write down your allergies and past reactions.
- Print two copies. Keep one in your wallet. Keep one at home.
- Update it the next time you get a new prescription.
That’s it. No apps needed. No fancy tools. Just a list. A simple, honest, updated list.
Final Thought
You don’t need to be a medical expert to keep your meds safe. You just need to be organized. And consistent. Your medication list isn’t about being perfect. It’s about being prepared. In a crisis, it’s the one thing you can control that could make all the difference.Do I need to include vitamins and supplements on my medication list?
Yes. Many people forget these, but they can interact with prescription drugs. For example, St. John’s Wort can reduce the effectiveness of birth control and antidepressants. Fish oil and garlic supplements can thin your blood, which is dangerous if you’re on warfarin. Always list them - even if you think they’re "natural" and harmless.
Should I carry my medication list with me at all times?
Yes. Emergency responders don’t have time to call your doctor. If you’re unconscious after a fall, accident, or heart issue, having your list on you - in your wallet, phone, or medical ID bracelet - can prevent deadly mistakes. Keep a printed copy and a digital backup.
What if I forget to update my list after a change?
Set a reminder on your phone for the day after every doctor’s visit or pharmacy pickup. If you’re on a new med, write it down the same day you get it. Outdated lists cause more errors than no lists at all. A 2023 AHRQ survey found that 100% of healthcare providers say immediate updates are critical.
Can my pharmacy help me create a medication list?
Yes. Most pharmacies can print a complete list of your prescriptions. Ask for it during your next refill. Some even offer free medication reviews with a pharmacist. Use that service - it’s free and can catch hidden interactions you didn’t know about.
Is it safe to use a smartphone app for my medication list?
Yes - if you use it correctly. Apps like MyMedSchedule and Medisafe are secure and FDA-approved. But don’t rely on them alone. Always carry a printed copy. Phones die, apps crash, and you might not have service in an emergency. Use apps as a tool, not your only backup.
How often should I review my medication list?
Review it every time you see a doctor, pick up a new prescription, or refill a medication. At minimum, do a full check every three months. If you’re on five or more drugs, do it monthly. The CDC recommends quarterly reviews for older adults and those with chronic conditions.






Swapneel Mehta
Been keeping a physical list since my dad had that bad reaction last year. Simple paper in my wallet, updated every time I get a new script. No apps, no fuss. Saved me when I passed out at the grocery store last winter - paramedics had the full list before they even hooked me up.
Stacey Smith
This is why America needs to stop letting people self-medicate with herbal nonsense. If you’re taking fish oil and warfarin, you’re playing Russian roulette with your organs. Stop pretending supplements are safe just because they’re ‘natural.’
Orlando Marquez Jr
It is imperative to acknowledge the systemic deficiencies in pharmacovigilance within the American healthcare infrastructure. The data presented herein underscores the critical necessity for patient-mediated documentation as a compensatory mechanism for institutional fragmentation. A standardized, universally accessible digital repository, interoperable across EHR platforms, would mitigate the majority of errors cited. Until such infrastructure is implemented, the burden remains disproportionately borne by the patient.
Jackie Be
I used to forget everything until I started taking pics of every bottle and saving them in a folder called MEDS DONT KILL ME 😭 now I never lose track even when I’m drunk at 2am and my phone dies
John Hay
My mom’s list saved her life when she went to the ER. She’s on 7 meds, 4 supplements, and a damn inhaler. The nurse didn’t know about the melatonin she took for sleep. They gave her a sedative. She almost stopped breathing. After that, I made her print two copies and give one to her neighbor. No excuses.
Jon Paramore
Per AHRQ guidelines, medication reconciliation errors account for 28% of preventable adverse drug events during care transitions. The inclusion of OTC agents and dietary supplements is non-negotiable - 61% of polypharmacy-related ER visits involve unreported OTCs. The pill photo method has demonstrated 94% concordance with pharmacy records in a 2023 JAMA study. Barcoded scanning reduces documentation lag by 63% in geriatric cohorts. Bottom line: compliance is non-optional.
Ben Warren
It is both irresponsible and profoundly negligent to suggest that a handwritten list is sufficient. The fact that this article even promotes paper as a viable solution reveals a dangerous lack of understanding regarding modern medical safety protocols. The CDC and FDA have explicitly endorsed digital, encrypted, cloud-synced systems with biometric authentication. To rely on a scrap of paper in your wallet is not just outdated - it is a moral failure. You are not merely risking your own life; you are endangering the entire healthcare ecosystem. If you cannot meet the baseline standard of digital literacy, you should not be managing polypharmacy.
Teya Derksen Friesen
I’ve been using the Medisafe app for three years now. It syncs with my pharmacy, sends reminders, and even alerts me when a new prescription might interact. I also keep a printed version in my purse - just in case. The combination of technology and redundancy is what makes this work. I wish more people understood that safety isn’t about effort - it’s about systems.
Sandy Crux
...and yet, despite all this... the article completely ignores the fact that most Americans cannot afford to refill their prescriptions regularly - let alone maintain a meticulously updated list. The real issue isn’t poor documentation - it’s a broken healthcare system that forces people to choose between insulin and groceries. A list won’t help if you’re skipping doses because you can’t pay for them. This is performative safety - a distraction from the real crisis.
Jason Silva
THEY’RE HIDING THE TRUTH 😱 your meds are being tracked by BIG PHARMA and the FDA app? it’s a spy tool!! 🤫 they use the barcode scans to build your health profile and sell it to insurers!! 🚨 i’ve got my list on a flash drive buried in my backyard with a note: ‘IF I’M DEAD, BURN THIS’ 🕵️♂️💊 #donttrusttheapp