Many older adults take five, ten, or even more medications every day. Some are for blood pressure, others for diabetes, arthritis, heart disease, or sleep. The pills come at different times - morning, noon, night, with food, without food, on an empty stomach. It’s easy to miss one. Or double up. Or forget why you’re taking it at all. This isn’t just confusing - it’s dangerous. Studies show that nearly half of older adults don’t take their meds as prescribed, and medication errors are a leading cause of hospital visits in people over 65.
Why Simplifying Medication Regimens Matters
It’s not about cutting pills. It’s about making life easier. When a person has to manage too many medications at too many times, their ability to stay on track drops fast. A 2020 study in Australia found that 83% of simplification efforts improved medication adherence. That means more people took their drugs when they were supposed to. But here’s the catch: better adherence doesn’t always mean better health. Taking the right pills at the right time helps, but it’s not a magic fix. The goal isn’t just to increase pills taken - it’s to reduce stress, confusion, and risk.
For many seniors, the real win is independence. If they can manage their own meds without help from family or nurses, they can stay in their homes longer. That’s why simplification is now a key part of geriatric care in Australia, the U.S., and across Europe. The Medication Regimen Simplification Guide for Residential Aged Care (MRS GRACE) was developed in 2020 to give healthcare workers a clear, step-by-step way to do this safely.
The Three Main Ways to Simplify
There are three proven methods to cut down on medication complexity - and they’re often used together.
- Fixed-dose combinations: Instead of two separate pills, use one pill that contains both drugs. For example, instead of taking a blood pressure pill and a water pill separately, a doctor might switch you to a single tablet that has both. This cuts pill count and reduces confusion.
- Once-daily dosing: Many medications come in long-acting forms. A statin for cholesterol can be taken at night. A blood pressure pill can be designed to last 24 hours. Switching from twice-daily to once-daily versions makes a huge difference.
- Combining both: The most effective approach reduces both the number of pills and the number of times you take them. For example, switching from four daily doses of three different drugs to two once-daily combination pills.
These aren’t just theory. A 2020 trial in the U.S. found that 41% of medication regimens for community-dwelling seniors could be simplified just by adjusting timing and switching to once-daily versions. In Australian aged care homes, pharmacists using the MRS GRACE tool were able to simplify regimens for 58% to 60% of residents.
What Works Best - and What Doesn’t
Not all drugs respond the same way to simplification. Some benefit hugely. Others don’t.
For insulin, simplifying to once-daily long-acting types helped seniors stick to their regimen - and even improved blood sugar control. For antipsychotics used in dementia, reducing frequency from twice daily to once daily lowered side effects and improved compliance.
But for blood pressure and diabetes meds, the results were mixed. In some cases, simplifying didn’t improve adherence at all. Why? Because timing matters. A statin works best at night. Thyroid medicine must be taken on an empty stomach, first thing in the morning. If you move those to match other meds, you might reduce confusion - but also reduce effectiveness.
That’s why simplification isn’t just about convenience. It’s about balance. As Dr. Sarah Hilmer from the University of Sydney says, “The clinical benefit of administering medications at a specific time of day may need to be balanced against the likely benefits achieved through reducing the overall regimen complexity.”
The 5-Step Process Behind Simplification
Good simplification doesn’t happen by accident. It’s a careful process. Here’s how it works in practice:
- Get the full picture: Start with a “best possible medication history.” This means gathering every pill, supplement, and over-the-counter drug the person is taking - from their doctor, pharmacy, and family. Studies show that on average, there are six errors or omissions between what the GP thinks the patient takes and what they actually take.
- Check if each drug is still needed: This is called deprescribing. Maybe that mild painkiller isn’t helping anymore. Maybe that sleep aid is causing falls. Removing unnecessary drugs is the first step to simplifying.
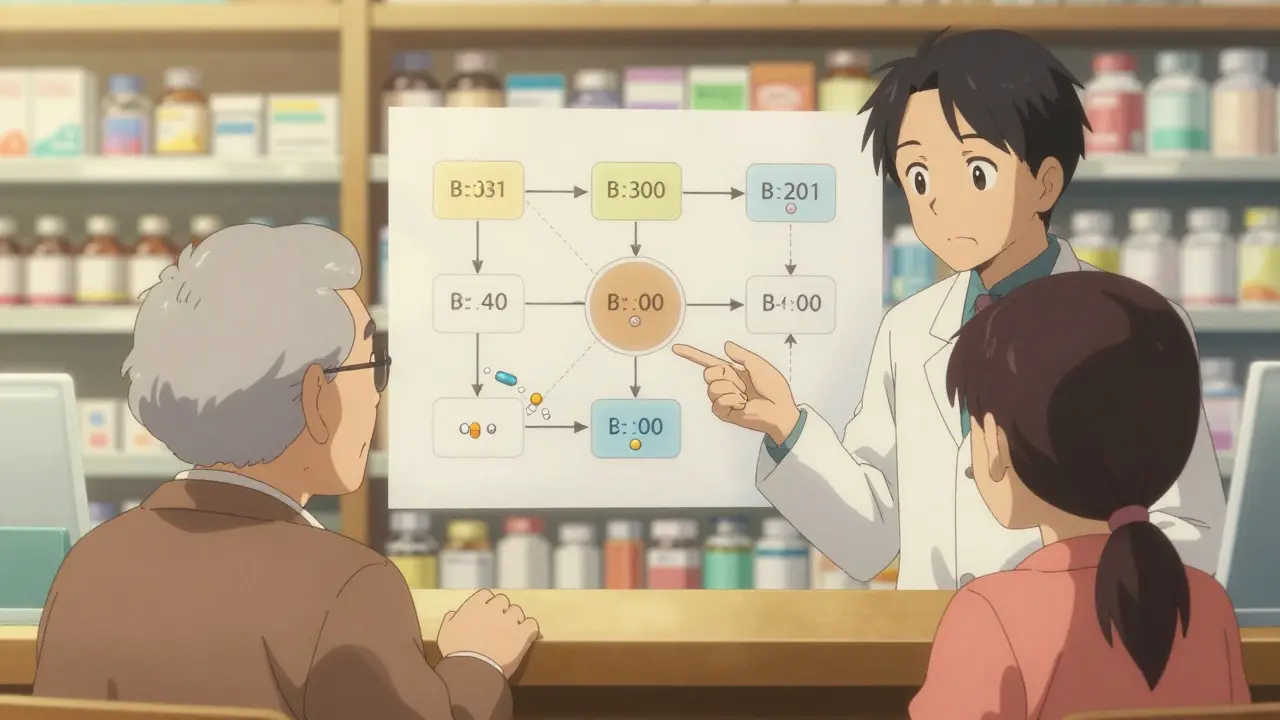
- Look for opportunities to combine: Are there two pills that can be merged into one? Are there versions that last longer? Pharmacists use tools like MRS GRACE to ask five key questions: Can the timing be aligned? Is there a combination product? Is there a once-daily alternative? Is the dose appropriate? Is there a safer option?
- Involve the person and their carer: Dr. Amy Theresa Page, who helped develop MRS GRACE, says simplification must include the patient’s preferences. Some people like to take their meds with breakfast. Others prefer evening. If you ignore that, they’ll stop taking them.
- Document and follow up: Changes need to be written down clearly. The pharmacy, GP, and caregiver all need updated lists. A follow-up in 4-6 weeks checks if the new plan is working.
In one Australian aged care facility, using this process led to a 30% drop in medication administration errors by staff. That’s not just safer - it’s less stressful for everyone.
Barriers to Implementation
Even though simplification works, it’s still not routine. Why?
First, it takes time. A full review with a pharmacist can take 45 to 60 minutes per person. Most GPs don’t have that kind of time. Second, many providers haven’t been trained. A 2023 survey found only 35% of pharmacy schools in Australia and the U.S. teach medication simplification as part of their geriatric curriculum.
Third, systems aren’t built for it. Electronic health records often don’t flag when a patient is on too many meds. Some tools, like Epic’s regimen complexity scorer (launched in 2022), are starting to help - but they’re not everywhere.
And then there’s the money. In Germany and parts of the EU, pharmacists get paid for doing these reviews. In Australia and the U.S., most of this work is unpaid or underfunded. That means it only happens when someone pushes for it - usually a concerned family member or a proactive pharmacist.
What Families and Caregivers Can Do
You don’t need to be a doctor to help. Here’s what you can do right now:
- Make a list of every medication - including vitamins, supplements, and creams. Include the dose and time.
- Take that list to the pharmacist. Ask: “Can any of these be combined? Can any be switched to once-daily?”
- Ask the doctor: “Is this drug still necessary?” Don’t be afraid to question a prescription.
- Use a pill organizer - but only if it matches the new schedule. A mismatch can cause more harm.
- Set reminders on a phone or tablet. Voice assistants like Siri or Alexa can be programmed to say, “Time for your blood pressure pill.”
- Check in weekly. Did they take their meds? Did they feel dizzy or tired after a change? Small changes matter.
One family in Sydney told us their 82-year-old mother was taking 12 pills a day. After a pharmacist review, they cut it to six - four of them once-daily combinations. The mom started taking her meds without reminders. She stopped falling. She said, “I feel like I’m in control again.”
The Bigger Picture
By 2050, the number of people over 65 will double worldwide. More seniors means more complex medication regimens. If we don’t fix this, hospitals will keep filling up with preventable errors.
Thankfully, change is coming. Australia now includes regimen simplification in its national Quality Use of Medicines framework. Medicare Advantage plans in the U.S. are starting to reward providers who reduce pill burden. The European Union has made it a priority for the next five years.
The future isn’t about more pills. It’s about smarter, simpler care. The tools exist. The evidence is clear. What’s missing is the will - and the time - to use them.
When Simplification Isn’t Safe
Not every change is a good idea. Some rules can’t be broken.
- Never stop a steroid suddenly - it can cause adrenal crisis.
- Don’t combine blood thinners without close monitoring.
- Don’t switch thyroid meds without checking TSH levels.
- Never change the timing of antiretrovirals - even a few hours off can cause resistance.
Simplification is not the same as cutting drugs. It’s refining them. Always work with a pharmacist or geriatrician. Don’t try to do it alone.







Annie Choi
Just had my grandma’s med review last week and wow-switched her from 11 pills to 5 once-daily combos. She’s sleeping better, no more dizzy spells, and actually remembers to take them now. No magic, just smart pharmacy work. Stop treating seniors like they’re broken and start treating their meds like they’re part of a life, not a chore.
Pharmacists are the real MVPs here. Let them do their job.
Dan Mack
They’re lying to you. Big Pharma doesn’t want you simplifying anything. Why? Because pills = profit. They push 12 meds because they own the patents. The ‘MRS GRACE’ guide? Written by consultants who get paid by drug reps. Your grandma’s ‘simplified’ regimen? Probably swapped one expensive combo for another that’s just as pricey. They don’t care if you live-they care if you keep buying.
Ask who funded the ‘studies.’ Always ask.
Sohan Jindal
This is why America’s going to hell. We let some foreign-trained pharmacist tell old people what to take. We used to respect our doctors. Now we let some guy with a clipboard cut pills like he’s playing Tetris. My uncle died because they took his heart med ‘for simplicity.’ That’s not simplification-that’s murder by bureaucracy.
Jaspreet Kaur Chana
Back home in Punjab, our elders take three herbs, one turmeric paste, and a cup of warm milk with honey-no pharmacy needed. But here? 15 pills at 5 different times. It’s madness. I saw my aunt cry because she couldn’t tell her blue pill from her green one. Why don’t we go back to simple? Food. Movement. Sleep. Not a drawer full of chemicals labeled in tiny print. We’ve forgotten how to be human.
Also-why is no one talking about how the system punishes people who can’t afford to pay for these pills? Simplify the system first, then the meds.
Niki Van den Bossche
Let’s be honest-the real tragedy isn’t the pill count. It’s the existential erosion. We’ve turned aging into a pharmacological audit. Every morning, a senior becomes a data point: compliance rate, adherence metric, polypharmacy score. Their dignity? Reduced to a pill organizer with 12 slots. The real innovation isn’t the combo tablet-it’s the quiet rebellion of someone who says, ‘I’m not a regimen. I’m a person who remembers the smell of rain on my mother’s porch.’
Stop optimizing. Start honoring.
Iona Jane
They’re watching you. Every time you use a pill organizer, every time you take a med at 8am sharp-they’re tracking you. The government, the insurers, the AI algorithms that predict your death based on your pill schedule. They don’t want you healthy. They want you predictable. That’s why they push ‘simplification’-so they can automate your care, your decline, your end-of-life costs. You think this is about helping? It’s about control.
ellen adamina
My dad took 14 meds. After the pharmacist reviewed them, they removed 5-none were actually helping. He’s 80. He didn’t need that sleep aid. He didn’t need that ‘preventive’ aspirin. He just needed someone to listen. I wish more people knew that sometimes the best medicine is saying, ‘You don’t have to take this anymore.’
Tom Doan
Of course simplification works. It’s not rocket science. But the fact that we need a 5-step guide to stop giving old people 12 pills a day says everything about how broken our healthcare system is. We’ve outsourced empathy to algorithms and called it ‘efficiency.’
Meanwhile, the guy who actually did the work-the pharmacist who spent 45 minutes with Mrs. Rivera-got zero reimbursement. That’s not a system. That’s a joke dressed in a white coat.
Amy Vickberg
This is why I love my pharmacist. She didn’t just cut pills-she asked my mom what she wanted to keep doing. Mom still takes her morning coffee and her one blood pressure pill together. That’s the win. Not fewer pills. More joy. We can fix this. We just have to choose to care.
And if you’re reading this and your parent’s on 10 meds-go to the pharmacy. Just go. Bring the list. Ask. It matters.
Nicholas Urmaza
Let me be clear. This isn’t about convenience. It’s about responsibility. If you’re a caregiver, a family member, or a clinician-you have an ethical obligation to question every prescription. Not because you distrust medicine-but because you respect life. The data is clear. Reducing unnecessary drugs reduces falls, reduces ER visits, reduces suffering. So why isn’t this standard? Because we’ve lost our moral compass. We optimize for cost, not care. Fix the system. Not just the pills.